Learning more about MTM during our Boston trip (July 21)
One of the highlights of our road trip north a few weeks ago was the visit to the Beggs Lab in Boston. In a way, going to the lab was the ultimate destination of our journey up the eastern seaboard. Though we knew that we weren’t going to come away with any major revelations, we also figured this would be the one time to take Lucas to the lab and meet some of the researches there before moving west.
So despite limited expectations, we were excited to walk into the lab on June 27 and meet the famous Alan Beggs. In fact, Dr. Beggs is a very gentle, thoughtful man (who’s really only famous in the world of children with severe muscle disease), and he invited us into his office for a long chat, ready to answer any and all questions we had for him. Dr. Beggs and the genetics counselor Elizabeth (who we had communicated with prior to the visit) were excited to meet Lucas, and it occurred to us that these researches probably didn’t have many opportunities to meet the wonderful children like Lucas who are affected by MTM.
The meeting started off with a bang: we laid Lucas down on Dr. Beggs nice couch and within minutes he had filled his shorts (after a 3-day hiatus from so doing!) and was gurgling with pleasure at the feat. Meanwhile, Dr. Beggs had launched into an overview of the different techniques being researched as possible treatments of myotubular myopathy.
First, he explained that they had already come along way in figuring out that the particular gene mutation seen in people with x-linked MTM affects the production of an enzyme called myotubularin. Lucas’s low muscle tone (and that of other people with MTM) results from the lack of myotubularin, which in turn prevents the proper development of muscle fibers. One thing we learned from Dr. Beggs and Elizabeth is that, based on the reading of Lucas’s DNA test for MTM, his body is probably not producing any myotubularin, whereas some kids with less severe forms of x-linked MTM do produce some of the enzyme. They were able to determine this because the test shows that the defective MTM gene is missing a pair of amino-acids. Since genetic information comes in triplets, missing a pair throws the entire sequence out of wack and likely means no myotubularin is produced.
Dr. Beggs explained the different directions of research for possible treatments. Their lab is looking into gene therapy, the technique we had heard most about, in which the mutated gene is replaced by a “good” gene mechanism. Researchers are trying to figure out how to deliver the new genetic information to all areas of the body, perhaps attaching the new genetic material to a virus to help it spread. The concept of gene therapy has been out there for a while but researchers are still far away from making it work – whether as a treatment for MTM or any other disease.
Researchers have also been working on a technique for infusing the blood with the missing myotubularin protein. It has been tested on mice with positive results and in recent years there has been excitement about finding a Labrador dog that also carries the MTM mutation to begin testing on. Still, the method is in the early stages of development and needs a lot more research before it could have potential with humans.
Another area of research involves helping the muscles grow in strength, despite the missing myotubularin. One possibility they’re pursuing is a muscle transplant-like procedure. A person would be given new muscle fibers, which would then reproduce using the stem cells of the non-MTM muscles. And finally, there are researchers looking into the possibility of giving muscles the capacity to grow bigger by inhibiting the action of an enzyme called myostatin that regulates our muscle growth. Apparently, animals who have this naturally occurring genetic disorder are able to grow enormous muscles. (Beggs showed us pictures of really enormous-chested dogs and cows.) If it worked, this kind of treatment might be useful not just to kids with MTM, but to people with other muscle diseases as well.
We knew we wouldn’t get any promises of treatments being available soon, and when we asked Dr. Beggs he walked the line of not giving us too much hope, but not dashing it, either. He said he didn’t think anything would be ready for trial on humans in less than 5-10 years. And he added that researchers gave a similar timeline for duchenne muscular dystrophy in the late 1980s, and yet they still haven’t found a treatment today.
The experience of being at the lab and in Boston was an important one for us and we left with a much better understanding of what Lucas’s disease is all about. But the conversations at the lab were scientific and “interesting,” not personal. It was only later, as we drove away, that we started to feel the heaviness of what we were learning.
Our belief has been that Lucas’s steady progress in terms of movement and strength will continue to be an upward curve. After the experience in Boston we’re now aware that might not be the case. Some boys who are on the more severe end of the MTM spectrum (as Lucas appears to be) have reached a peak at a young age in terms of strength and movement. As their bodies got bigger and heavier to lift they’ve encountered more challenges, like having a hard time interacting and communicating without augmentative devices. It’s scary to hold the possibility that all the amazing steps Lucas taken – especially in terms of his ability to use his arms and express himself through sign language – may not continue to expand. In fact, scary is an understatement. It’s downright awful, at times, to think about the future and the fact that Lucas could face even more physical barriers than he does now.
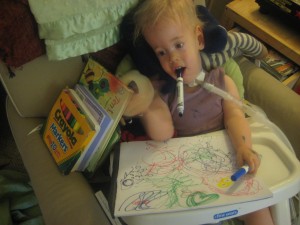
Of course, by the time we got home we were back to our regular routine of enjoying hanging out with Lucas and all his brilliance, goofiness, fussiness, challenges and strengths. We continue to get excited about all the progress he makes with sign language, physical development, and everything else. Celebrating Lucas for who he is in the present remains our guiding philosophy, even if new knowledge sometimes makes us nervous about the future.