Understanding the tracheostomy (Oct. 21)
On Monday afternoon we changed Lucas’s trach for the first time. We had received a 2-hour long workshop last week, and had performed a trach change on a cabbage-patch doll, but this was the real thing. 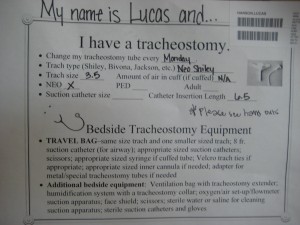 It went fine, and now that we’re feeling confident enough about our ability to take care of Lucas’s trach we figured we’d elaborate on what it’s all about.
It went fine, and now that we’re feeling confident enough about our ability to take care of Lucas’s trach we figured we’d elaborate on what it’s all about.
Before Lucas’s surgery we explained why the doctor’s recommended a tracheostomy for him (see “Gettting ready for surgery”). Basically, the muscles in his upper airway are still too weak to hold his throat open wide enough to breath effectively on his own through his nose and mouth. Since Lucas continues to get stronger we’re confident that his trach is a temporary step, but it’s also a commitment: once the surgery is done they expect a child to have the trach for at least 3-4 month before considering removing it. As we mentioned the other day Lucas is doing great on his breathing, and he probably won’t even need the ventilator after a while (we’ll test him off the vent, on a “trach collar”, before we leave the hospital). But still, the trach is going to be a part of his life, and therefore our lives, for a while so we’re doing all we can to learn how it works.
 The trach itself is a small piece of hard plastic that fits into Lucas’s stoma (the hole in his neck made by the surgeon ). It becomes his principal airway, though because there is a small leak he’s also able to do some breathing around the trach through his nose and mouth. It occasionally gets clogged up with mucus, so one of the things that we’ve learned to do over the last week is suction out the trach using a small, sterilized catheter suction tube.
The trach itself is a small piece of hard plastic that fits into Lucas’s stoma (the hole in his neck made by the surgeon ). It becomes his principal airway, though because there is a small leak he’s also able to do some breathing around the trach through his nose and mouth. It occasionally gets clogged up with mucus, so one of the things that we’ve learned to do over the last week is suction out the trach using a small, sterilized catheter suction tube. 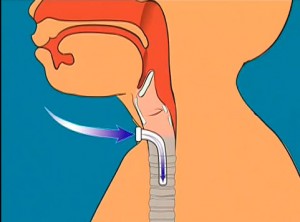 Sterility is very important since the trach is a much more direct access-point to Lucas’s lungs. Therefore, we also need to clean a couple times a day around the stoma and replace the “trach ties” (which hold the trach in place and sometimes get sweaty). All of these procedures are complicated by the fact that Lucas is still connected to a vent, the tubing of which can pop off the trach at any time if we’re not careful.
Sterility is very important since the trach is a much more direct access-point to Lucas’s lungs. Therefore, we also need to clean a couple times a day around the stoma and replace the “trach ties” (which hold the trach in place and sometimes get sweaty). All of these procedures are complicated by the fact that Lucas is still connected to a vent, the tubing of which can pop off the trach at any time if we’re not careful.
Already the nurses have pretty much turned over the duties of Lucas’s trach care to us, though they do keep an eye on our technique and make recommendations. The big step was the aforementioned trach change, which involves actually removing the trach itself (which Krista did) and placing a new one in its place (which Burke did). The trach IS what allows Lucas to breath, so if something were to go wrong during that process then he would go into distress. Of course, that’s why there are also emergency items on hand, such as a smaller size trach and most importantly, the “bag” which allows us to get oxygen to Lucas if he stops breathing on his own or something temporarily clogs his airway.
For those that want to know more, you can check out this good, long description of all that goes into trach care. And below you can watch a couple clips from a cheesy video that made by Shiley, the brand of trach that Lucas wears. The second part shows all the items we’ll need to carry along with us when we take Lucas for a walk in the park (we just picked up a stroller that accommodates his car seat and has a hefty compartment for storing items on those journeys out of the house.)


Comments (1)
Chartese
November 16th, 2009 at 1:21 pm
Hi Burke and Krista,
I am so sorry I did not get a chance to say goodbye before you and Lucas headed home. The amazing thing is that he is home and will sail right through to a healthy recovery.
We should definitely keep in touch as our little ones continue to grow and defy the odds showing everyone the true miracles that they are.
Feel free to contact me anytime and also let me know how Lucas is doing.
All the best,
Chartese
(Amaris’ mom)
202.386.0700 (cell)
chartese.d.day@gmail.com
Leave a reply